Small Cell Lung Cancer
Small cell lung cancer (SCLC) is the second-most common type of lung cancer. Though it’s more aggressive than non-small cell lung cancer (NSCLC), treatments may allow SCLC patients to live longer or even become survivors. Learn more about this type of lung cancer and how Lung Cancer Group can help qualifying SCLC patients get compensation for treatments and other expenses.
What Is Small Cell Lung Cancer?
Small cell lung cancer is one of the main types of lung cancer, accounting for 10% to 15% of all cases.
SCLC typically forms in the lung’s airways before quickly spreading to other parts of the body.
While SCLC is often not diagnosed until it has already spread, treatments can help many patients live longer. Some patients may become cancer-free with medical care.
It’s crucial to consider quickly getting diagnosed if you or a loved one could have SCLC as a result — the sooner it’s detected, the faster treatments can start.
- Between 23,000 and 35,000 people are diagnosed with SCLC in the U.S. each year.
- Commonly used treatments for SCLC include chemotherapy, radiation, and immunotherapy.
- SCLC patients live for 7 months on average, but some patients have lived for 30+ years thanks to the treatments they received.
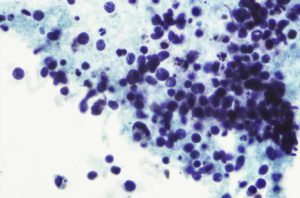
- This type of lung cancer is sometimes called oat cell cancer as its tiny, round cells resemble oats under a microscope.
Get our Free Lung Cancer Guide to learn more about SCLC, available treatment options, and compensation.

- Understand risk factors
- Find top treatments
- Pursue compensation
What Causes Small Cell Lung Cancer?
The most common cause of SCLC is cigarette smoking, according to leading cancer organizations like the American Cancer Society (ACS) and Yale Medicine.
“It’s very rare for someone who has never smoked to have SCLC. The risk for lung cancer among smokers is many times higher than among non-smokers. The longer you smoke, and the more packs per day you smoke, the greater your risk.”
— American Cancer Society
People can also develop SCLC if they are exposed to secondhand smoke, radon, asbestos, and other cancer-causing chemicals.
Small Cell Lung Cancer and Asbestos Exposure


Breathing in asbestos fibers can cause SCLC and other cancers 10-50 years later. Smokers are at an even higher risk as asbestos worsens the lung damage caused by cigarette smoke.
Many cases of SCLC linked back to asbestos could have been avoided as manufacturers of asbestos-containing products knew the dangers as early as the 1930s. But instead of warning the public, these companies hid the risks for decades to continue to profit while people got sick.
At Lung Cancer Group, we find the negligence of these asbestos companies unacceptable. Let us help you pursue justice and compensation for SCLC right now: Get a free case review.
Small Cell Lung Cancer Symptoms
- A cough that won’t go away or gets worse
- Bloody mucus coughed up from lungs (sputum)
- Chest pain
- Difficulty breathing and swallowing
- Fatigue
- Hoarseness
- Loss of appetite
- Shortness of breath
- Swollen face and/or neck veins
- Weight loss
These symptoms are the same as other types of lung cancer, like NSCLC, according to the National Institutes of Health (NIH).
The National Cancer Institute (NCI) encourages you to see a doctor if you have any lung cancer symptoms. Doctors can find out if your symptoms are caused by lung cancer and help you get treatment.
Small Cell Lung Cancer Diagnosis
To diagnose SCLC, your doctor will first note down what symptoms you have. They may also ask if you have ever smoked or were exposed to other toxins like asbestos.
From there, your doctor can use imaging scans to look inside your body for growths or masses that could be lung cancer tumors.
Imaging scans used to help diagnose SCLC include:
- CT (computed tomography) scans
- PET (positron emission tomography) scans
- MRI (magnetic resonance imaging) scans
- X-rays


Imaging scans alone won’t be enough to diagnose SCLC, though. Your doctor will order a biopsy if they think you have cancer after these tests.
Through a biopsy, the doctor takes out a small sample of tissue or fluid from a part of the body that may be cancerous using a bronchoscopy (a small tube with a camera at the end) or a needle.
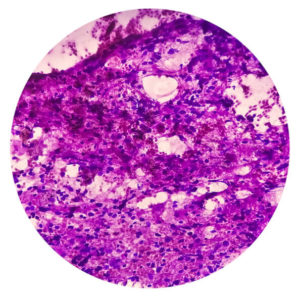
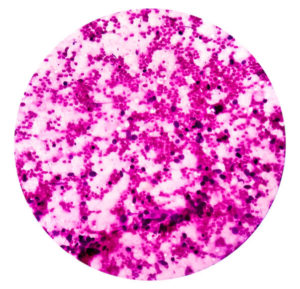
The sample is then sent to a lab, where it will be looked at under a microscope to see which type of lung cancer cells (if any) are present.
You are highly encouraged to get regular lung cancer screenings and promptly see a doctor if you develop any symptoms. Both of these may help catch SCLC before it spreads far.
Small Cell Lung Cancer Stages
There are two stages of small cell lung cancer: the limited stage and the extensive stage. The stage you are diagnosed in can greatly impact your overall health outlook and treatment plan.
Doctors can determine which stage of lung cancer you have at the time of diagnosis.
Limited-Stage Small Cell Lung Cancer
In cases of limited-stage SCLC, the cancer hasn’t spread throughout the body.
Tumors are found in:
- The lung where the cancer started
- The lung and nearby lymph nodes in the collarbone and the mediastinum (space between lungs)
Sometimes, only one tumor is found, allowing doctors to remove the cancer through surgery. Around 33% of SCLC patients will be diagnosed in the limited stage, according to the American Society of Clinical Oncology (ASCO).
Extensive-Stage Small Cell Lung Cancer
Extensive-stage SCLC has spread past the lung and into other parts of the body. This spread is known as metastasis.
By this stage, tumors may have reached:
- Bones and bone marrow
- Liver
- Brain
- Other organs far away from the lungs
Roughly 66% of SCLC patients are diagnosed in the extensive stage because many patients don’t have worrisome symptoms until the cancer has spread. This stage is also harder to treat than the limited stage.
Get a Free Lung Cancer Guide to learn more about the different SCLC stages and how to access treatments to live longer.




- Understand risk factors
- Find top treatments
- Pursue compensation
Subtypes of Small Cell Lung Cancer
There are two subtypes of SCLC, according to the World Health Organization (WHO). Doctors determine which subtype a patient has by examining the cells they see during a biopsy.
![Combined Small Cell Lung Carcinoma]()
Combined Small Cell Lung Carcinoma
Combined small cell lung carcinoma (C-SCLC) is when a patient’s tumors have both small cells and cells from one or more types of NSCLC.
C-SCLC cases account for anywhere from 5% to nearly 30% of all SCLC cases, according to a review of various studies published in OncoTargets and Therapy.
![Small Cell Carcinoma]()
Small Cell Carcinoma
Small cell carcinoma is the most common subtype of SCLC, according to the Mount Sinai Health System.
In this type, tumors are solely made up of small cells. It is also known as oat cell carcinoma.
Small Cell Lung Cancer Prognosis
A prognosis is the expected outcome of a particular disease. Generally speaking, the prognosis for SCLC is poor as most patients are diagnosed after the cancer has spread, limiting treatment options.
That said, some patients can live much longer. Unique patient factors can greatly affect an SCLC prognosis.
These factors include:
- Age: Younger patients will likely be in better health besides having cancer, allowing doctors to try more aggressive treatments to destroy as much of the cancer as possible.
- Cell type: Patients with C-SCLC who qualify for surgery may have a better prognosis than patients with small cell carcinoma (who usually cannot get surgeries).
- Overall health: Patients without other pre-existing health problems may better tolerate medical treatments and their side effects.
- Stage of the cancer: Limited-stage SCLC patients have a better health outlook than those with extensive-stage SCLC, as there are more treatment options for limited-stage patients.
Prognosis is often measured using two factors: life expectancy and survival rate.
Small Cell Lung Cancer Life Expectancy
Life expectancy is how long a doctor believes a patient will live. Patients with SCLC often face a short life expectancy.
- Limited-stage SCLC patients have a life expectancy of 18 to 23 months
- Extensive-stage SCLC patients live for 8 to 10 months on average
Further, the overall SCLC life expectancy was 7 months in a 30-year study of SCLC patients by the Surveillance, Epidemiology, and End Results (SEER) registry.
Small Cell Lung Cancer Survival Rate
Survival rate is the percentage of patients still alive after a set time period. It’s typically measured in years and given as a percentage.
Here are the average SCLC survival rates from the Cleveland Clinic:
- The 5-year survival rate for limited-stage SCLC is 20%
- The 5-year survival rate for extensive-stage SCLC is 3%
That said, life expectancies and survival rates are averages, and you may be able to outlive your initial SCLC prognosis with the right cancer care plan in place.
Call (877) 446-5767 to learn how you can afford treatments to improve your SCLC prognosis.
Surviving Small Cell Lung Cancer
Some people diagnosed with small cell lung cancer have gone on to become cancer-free or live much longer than expected thanks to medical treatment. These patients are considered lung cancer survivors.
Notable SCLC survivors include:
- Nina, 10-year survivor: Nina was diagnosed with SCLC in 2014 following a routine scan, which caught the cancer in a limited stage. She underwent chemotherapy and radiation and later joined an immunotherapy trial, which has kept her symptoms at bay.
- Toni, 30+ year survivor: Toni’s diagnosis came in 1992 after an initial misdiagnosis of tuberculosis. Following long-term treatment, which included chemotherapy and numerous radiation sessions, Toni became cancer-free.
- Montessa, 18+ year survivor: In 2006, Montessa’s world changed forever when she was diagnosed with SCLC at the age of just 28. She was treated with chemotherapy and radiation and has been cancer-free ever since. She now works to raise awareness about lung cancer to help other patients.
Even if your lung cancer prognosis is poor, don’t lose hope. You can still become an SCLC survivor with help from a dedicated cancer care team.
Small Cell Lung Cancer Treatment Options
Getting treatment is the best way for patients with small cell lung cancer to live longer.
Your SCLC treatment plan may include:
- Chemotherapy
- Immunotherapy
- Radiation
- Surgery (in some cases)
“Lung cancer is treatable, no matter the size, location, whether the cancer has spread, and how far it has spread.”
— American Society of Clinical Oncology (ASCO)
Learn about small cell lung cancer treatments doctors may use to help you or a loved one below.
Chemotherapy
Doctors administer chemotherapy (cancer-killing medications) to kill SCLC cells and shrink tumors. Chemotherapy is the most common treatment for SCLC, according to Johns Hopkins Medicine.
Chemotherapy drugs destroy cancer cells throughout the body, not just in the lungs. This makes chemotherapy a key treatment for SCLC patients, as most are diagnosed after the cancer has spread.
Several chemotherapy drugs can be used to treat SCLC, including:
- Cisplatin
- Carboplatin
- Etoposide
Doctors often use several types of chemotherapy at once in what’s known as a regimen for best results.
“SCLC is highly responsive to chemotherapy and sometimes improvement can be rapid and dramatic. However, cancer often returns and may become resistant to the chemotherapy regimen that was successful in the past.”
— National Organization for Rare Disorders (NORD)
Doctors can also modify a chemotherapy regimen if a patient’s cancer doesn’t respond to it or comes back after treatment.
Get a Free Lung Cancer Guide to learn more about how treatments like chemotherapy can help improve your SCLC prognosis.




- Understand risk factors
- Find top treatments
- Pursue compensation
Immunotherapy for SCLC
Cancer cells can sometimes hide from the immune system. Immunotherapy medications boost the patient’s immune response to find and destroy cancer cells.
Two immunotherapy medications have been approved to treat SCLC: Tecentriq (atezolizumab) and Imfinzi (durvalumab). Both are immune checkpoint inhibitors, which specifically prevent cancer cells from hiding from the immune system.
Immunotherapy is often combined with chemotherapy to treat SCLC and help patients live longer, according to the ACS. Using multiple treatments together allows more of the cancer to be destroyed.
Radiation Therapy
Doctors use radiation (energy beams similar to X-rays, but much stronger) to destroy cancer cells and shrink tumors.
There are several types of radiation therapy for lung cancer. The most commonly used type to treat SCLC is called external beam radiation therapy (EBRT).
EBRT involves giving radiation through a machine. An SCLC patient typically will undergo several EBRT sessions during the course of their treatment.
Besides its use as a main treatment, radiation can also be used:
- During/after chemotherapy treatments
- On the brain to prevent SCLC from spreading there
- To reduce cancer symptoms
Radiotherapy itself is painless, but it can lead to side effects like hair loss, tiredness, and nausea. Check with your doctor ahead of time so you are aware of any possible side effects.
Surgery


Doctors may perform surgery if there’s only one lung tumor found during a diagnosis, as with it all of the cancer can be removed.
Doctors will then recommend follow-up treatments like chemotherapy after surgery to ensure that the cancer doesn’t return.
The ACS notes that only 5% of SCLC patients can undergo surgery. This is because most SCLC patients will be diagnosed after the cancer has spread through their bodies, and thus, surgery won’t help them live longer.
Clinical Trials
Cancer research programs are conducting clinical trials to test new and possibly more effective SCLC treatment options. Depending on the unique factors in an SCLC patient’s case, they may qualify to join a trial.
SCLC clinical trials are studying:
- Chemotherapy, targeted therapy, and immunotherapy: A recent study combined a targeted drug called olaparib, an immunotherapy drug known as cediranib, and chemotherapy to help SCLC patients live longer. Chemotherapy kills cancer cells, while the other drugs block enzymes on the cells so they can’t grow or divide.
- Radiation and immunotherapy: In the ongoing RAPTOR trial, researchers are comparing how patients respond when radiation therapy is used alongside the immunotherapy drug Tecentriq. They want to see if the combination will prevent SCLC from growing compared to just using immunotherapy.
- Stereotactic radiosurgery (SRS): This trial is looking at how SRS could help SCLC patients whose cancer has spread to the brain. SRS allows doctors to precisely target tumors while sparing the brain itself.
Reach out to your lung cancer health care team if you’re interested in joining an SCLC clinical trial.
Other Small Cell Lung Cancer Treatment Options
Besides the SCLC treatments listed above, doctors may sometimes use other lung cancer treatments to help patients.
Additional SCLC treatments include:
- Pain-relieving medications: These drugs are used to reduce cancer symptoms and side effects of other treatments.
- Stent placement: Doctors place a short tube into an airway that’s blocked by cancer cells so patients can breathe more easily.
- Supplemental oxygen: This can also help improve a patient’s breathing.
How effective these treatments are depends on the unique nature of your case. Talk with your doctor about the best options for you.
Compensation for Small Cell Lung Cancer
SCLC patients may qualify for financial compensation following a diagnosis if their cancer is linked back to corporate negligence.
For example, private companies knew that asbestos could cause SCLC and other cancers but used products with the substance anyway for decades.
You or a loved one may be able to get compensation if you were exposed to products made by these companies and now have SCLC, even if you smoked.
Many past lung cancer patients we’ve helped have secured $1 million or more in compensation through the options listed below.
SCLC compensation options include:
- Lawsuits: Through a lung cancer lawsuit, you can secure compensation and justice from manufacturers of asbestos-containing products. A skilled lung cancer lawyer can walk you through each step of the process.
- Trust funds: Dozens of asbestos companies filed for bankruptcy to avoid lawsuits, but they were forced to set up asbestos trust funds to pay victims. With help from a lawyer, you may qualify to access some of the estimated $30 billion available in these trusts.
- VA benefits: Many military veterans were put at risk of lung cancer due to service-related asbestos exposure. As a result, these veterans can file for VA benefits to get monthly financial payouts and free or low-cost medical care.
Get a free case review now to learn about all the lung cancer compensation options that you may qualify for.
- Access Financial Aid and Justice
- Learn About Your Options
- Contact Us for Free


We Can Help Small Cell Lung Cancer Patients
Being diagnosed with small cell lung cancer — or any type of cancer — is devastating. While SCLC is a less common and more aggressive form of lung cancer, there is hope.
When facing an SCLC diagnosis, remember the following:
- Doctors across the country treat SCLC
- Lung cancer treatments can help you live longer and ease pain
- Other SCLC patients have become long-term survivors
“Sometimes people hear the word ‘cancer,’ and they immediately still think it’s a death sentence. Cancer care has moved way beyond that now.
— Nina, 10-year SCLC survivor
At Lung Cancer Group, we’ll stand by you throughout your cancer fight. We can help you learn more about your cancer diagnosis and pursue financial compensation to cover your medical costs and any other expenses if you’re eligible.
Don’t wait: Call (877) 446-5767 or get a Free Lung Cancer Guide now to see how we can help after an SCLC diagnosis.
Small Cell Lung Cancer FAQs
What is the survival rate for small cell lung cancer?
SCLC has a low average survival rate since it’s very aggressive, and most patients are diagnosed only after it has spread. The overall 5-year survival rate for SCLC patients is just 7%, according to ASCO.
However, it’s possible that you could live for many years depending on how your body responds to treatment, how far the cancer has spread by the time of your diagnosis, and more.
How curable is small cell lung cancer?
While there’s no official cure for lung cancer (or any type of cancer), some patients may be considered “cured” if their body responds well to treatment.
“Cured” SCLC patients won’t have any symptoms and can live their lives normally.
Talk to your doctor about cancer care options that can help you live longer or potentially cure your SCLC.
How aggressive is small cell lung cancer?
Small cell lung cancer is generally more aggressive than other types of lung cancer. How aggressive your case is depends on how far it has spread at the time of diagnosis and if doctors can easily treat it or not.
Call (877) 446-5767 now to learn if you qualify for compensation that can help you afford medical treatments for SCLC.
How fast does small cell lung cancer spread?
SCLC spreads very quickly. According to a series of studies analyzed in a report from Clinical Medicine Insights: Oncology, SCLC tumors can double in size in anywhere from 25 to 217 days.
Thankfully, SCLC also shrinks rapidly after treatments like chemotherapy and radiation, according to Yale Medicine.
Has anyone beat stage 4 small cell lung cancer?
Technically, SCLC is only classified into two stages: limited and extensive. The extensive stage roughly correlates to a stage 4 NSCLC diagnosis.
With all that said, some people diagnosed with extensive-stage SCLC have gone on to live for many years after a diagnosis.
Ina was shocked when she was diagnosed with extensive-stage SCLC in 2006. However, she was determined to fight. Thanks to chemotherapy and outpatient treatments, Ina became a long-term survivor.
Get a Free Lung Cancer Guide now to find treatments for stage 4 small cell lung cancer.
Who’s at risk of small cell lung cancer?
The biggest risk factor for small cell lung cancer is smoking cigarettes or other tobacco products. Most people diagnosed with SCLC are either former or current smokers.
Further, you’re at a high risk of any type of lung cancer — as well as other asbestos-related diseases like mesothelioma — if you regularly worked with or around asbestos-based products.
You are encouraged to get lung cancer screenings if you regularly smoked but don’t have lung cancer. Doing so can help doctors possibly catch cancerous tumors before they spread.
Can small cell lung cancer be caused by asbestos exposure?
Yes. You could develop small cell lung cancer if you were exposed to asbestos fibers and the fibers got stuck inside your lungs.
Asbestos fibers damage healthy lung tissue and can cause SCLC tumors to form decades later.
Asbestos exposure can also cause any other type of lung cancer, as well as mesothelioma (a cancer of the lining of major organs), asbestosis (a noncancerous illness that weakens the lungs), and other diseases.
Can small cell lung cancer be prevented?
While there’s no way to fully prevent any type of cancer, you can significantly lower your risk of SCLC by taking preventative steps.
Arguably, the best way to prevent SCLC is to not smoke or quit as soon as possible. NYU Langone Health notes that the main cause of SCLC is smoking cigarettes.
Avoiding other cancer-causing materials like asbestos or radon can also help prevent SCLC.